Diabetes is a chronic condition that affects the whole body. If left uncontrolled, it can cause many life-threatening complications such as severe, spreading infection leading to the need for multiple segmental amputations. Diabetic patients must consult a podiatrist regularly to maintain the health of the lower legs and prevent any further damage to the feet and legs that could lead to amputation.

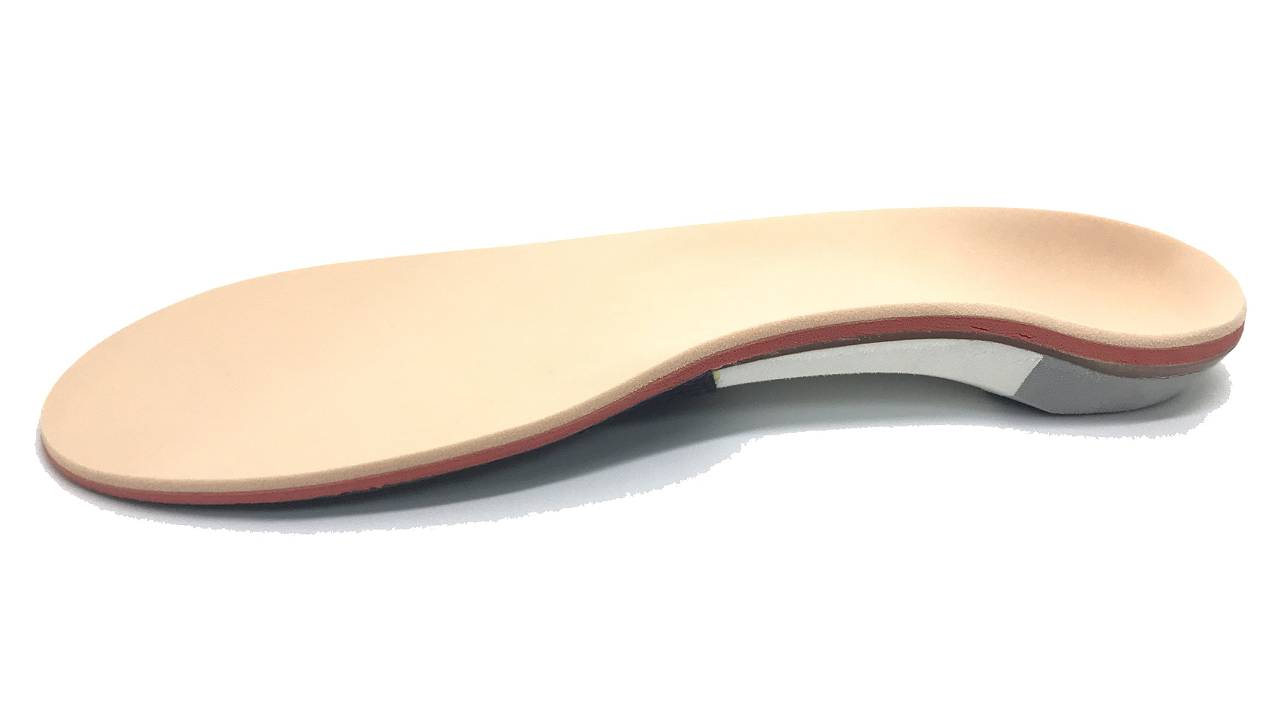
Off the shelf standard foot orthotics that come without a prior assessment or prescription are not recommended for the diabetic foot. Foot orthotics for diabetic patients are different to ordinary insoles and are precisely designed to support the patient’s specific, complex, and changing foot structure. The footbed of a diabetic orthotic must contour exactly to the patient’s foot and allow for normal foot function without hindrance. This prevents high-pressure areas from becoming callused and eventually breaking down into diabetic wounds.
The foot is subjected to pressure and shearing forces during walking.
For diabetic patients, using any form of intervention under the foot can be considered a high-risk approach, as the wrong device can potentially cause more issues. The process of dispensing diabetic orthotics often needs to be closely monitored with regular follow-ups so the necessary adjustments can be made as the condition progresses.
Diabetic Orthotics
Diabetic orthotics must be customised in consideration of the diabetic patient’s current foot shape and biomechanics, along with underlying bone, joint, and soft tissue disorders that are associated with the high-risk diabetic foot. Diabetic orthotics should be specifically designed to address the underlying biomechanical changes of the foot and leg while reducing shearing and frictional forces that contribute to skin breakdown and infection.
Along with specifically designed diabetic orthotics, the diabetic patient must also take care to wear the correct footwear for their foot and ankle condition. Podiatrists specialise in understanding the appropriate footwear designs and features a diabetic patient requires to reduce the risk of amputation.
Diabetic patients should keep an eye out for these features when looking for orthotic-suitable footwear:
- A smooth inner lining
- Secure fastenings around the midfoot and ankle
- A supportive and cushioned base
Flatfoot in Diabetic Patients
Patients with uncontrolled diabetes and neuropathy may not be able to feel when there is excessive pressure on their feet due to the loss of sensation. This pressure is often accompanied by reduced blood supply to the foot, causing the bones to soften and shift. When soft tissues and foot joints become destroyed, fluid can accumulate and deform the foot in an extremely short amount of time.

The presence of flatfoot in a diabetic patient can be highly concerning as it may be a misdiagnosed case of Charcot foot, which is a serious diabetic foot complication that requires prompt medical attention.
Symptoms of Charcot foot:
- Warm to the touch
- Redness
- Swelling
- Pain or soreness
In some cases, patients who do not present with any symptoms and continue walking on their feet without being aware of their condition can suffer bone fractures due to unrelenting pressures on their feet. Deformities in any part of the foot can also result in skin ulcers due to any bone protrusions that press against the ground or inside the shoes. Ulcers are often difficult to heal due to diabetic complications and can even become infected, which may require amputation in severe cases.
Our podiatrists will usually prescribe a walking cast or a boot and advise patients to minimise walking. Once out of the boot, our podiatrists will prescribe custom diabetic orthotics to support the foot and prevent further deformity. Severe cases of Charcot foot may require bone reconstruction surgery.
There are two main areas that podiatrists focus on:
1. Motor (muscle)
Insufficient insulin and a rise in blood sugar levels will result in the inability of muscle cells to grow and thrive. This can cause severe muscle loss and reduce overall strength in the muscles, most significantly in the lower limbs, causing gait and balance to become altered. This can result in impaired motor abilities and an increased risk of falls which can be highly dangerous for elderly individuals.
2. Sensory
The nervous system is vast and runs from your head to your toes. It is in charge of regulating your muscles (skeletal, vital organs, eyes, etc) and everything to do with your skin (sweating, sensation).
-
Peripheral Arterial Disease
Too much blood glucose (sugar) can cause irreversible damage to your nervous system, contribute to reduced blood flow, and increase the risk of high cholesterol and high blood pressure. Limited blood flow in the lower limbs can also lead to pain during walking that abides with rest, an easily identifiable symptom of Peripheral Arterial Disease (PAD). Patients suffering from PAD have a high chance of developing gangrenous wounds due to the lack of nutrients and oxygen, which can lead to subsequent amputation-causing infections.
-
Diabetic neuropathy
Diabetic neuropathy is the result of nerve damage caused by high sugar build-up in the compact spaces of organs. When nerves are damaged, signals sent to the brain become obstructed and the nerves may eventually stop communicating with the brain as a whole. Damage to the large sensory fibres is long-term, resulting in the diabetic patient having reduced sensations to vibrations and touch, while damage to the small sensory fibres causes the individual to be unable to distinguish hot and cold temperatures, or feel itchiness or pain in their feet.
3. Physical
Due to the reduction in sensory feelings, a diabetic patient can suffer serious wounds without even being aware of them. These can deteriorate unknowingly and develop infections, which are a major risk factor for limb amputations and loss of life.
-
Foot deformities
Nerve damage can cause immense pain and foot deformities such as hammer, claw, and mallet toes, high arches, extreme flatfoot (Charcot foot), and bunion development, leading to high-pressure areas across the feet. Coupled with the lack of sensation resulting from neuropathy, a patient can easily develop undetected ulcers and wounds.
-
Reduced immunity to infections
If wounds develop (due to increased pressure or injury), increased sugar in the blood encourages the growth of bacteria and can impair the function of white blood cells. This impacts the healing rate of wounds and slows down the body’s ability to fight infection. The longer they go without proper care, the higher the risk of infections as well.
Even a small fungal infection may enter your skin and become a rapidly spreading soft tissue infection or develop into a serious condition known as sepsis. Patients with long-term uncontrolled diabetes may need surgical intervention to improve circulation, remove infected tissue, or amputate areas of dead tissue.

Diabetic patients are advised to go for annual diabetic foot screenings to check for any signs of nerve damage, loss of sensation, and undetected diabetic wounds and ulcers. Your podiatrist will conduct a blood flow assessment and provide regular reminders on diabetic foot care. Routine nail trimming and debridement services on diabetic feet should only be performed by qualified podiatrists when required.

- Schedule yearly check-ups with your podiatrist
- Check your feet daily and use a mirror for hard to reach places
- See your podiatrist if you are having foot problems
- Regulate your blood sugars, with help from a doctor and dietician if needed
- Wash and dry your feet thoroughly daily, especially between the toes
- Avoid soaking your feet, this dries out the skin causing your skin barrier to weaken
- Use moisturising cream daily to help soften your skin
- Avoid putting creams between your toes as this can increase bacterial and fungal growth
- File/trim your toenails if they are visible and accessible
- Wear supportive footwear outdoors
- Wear cushioned and supportive sandals at home
- Choose the right footwear
- Buy footwear at the end of the day to accommodate for foot swelling
- Break-in new shoes slowly
- Keep active to promote circulation
- Quit smoking




