Arthritis is a term used to describe inflammation around one or more of your joints. This leads to pain, stiffness and erosion of the joint in question. There are over a hundred different types of arthritis, but the most common form is osteoarthritis. Osteoarthritis is common amongst the aged population, typically those over the age of 60. While the term ‘rheumatism’ is rarely used by healthcare professionals today, it is still frequently used by the general public to describe arthritic conditions that involve wear and tear of a joint or body part.1 Although osteoarthritis often presents itself in the knees, it can also occur in the ankle and foot.
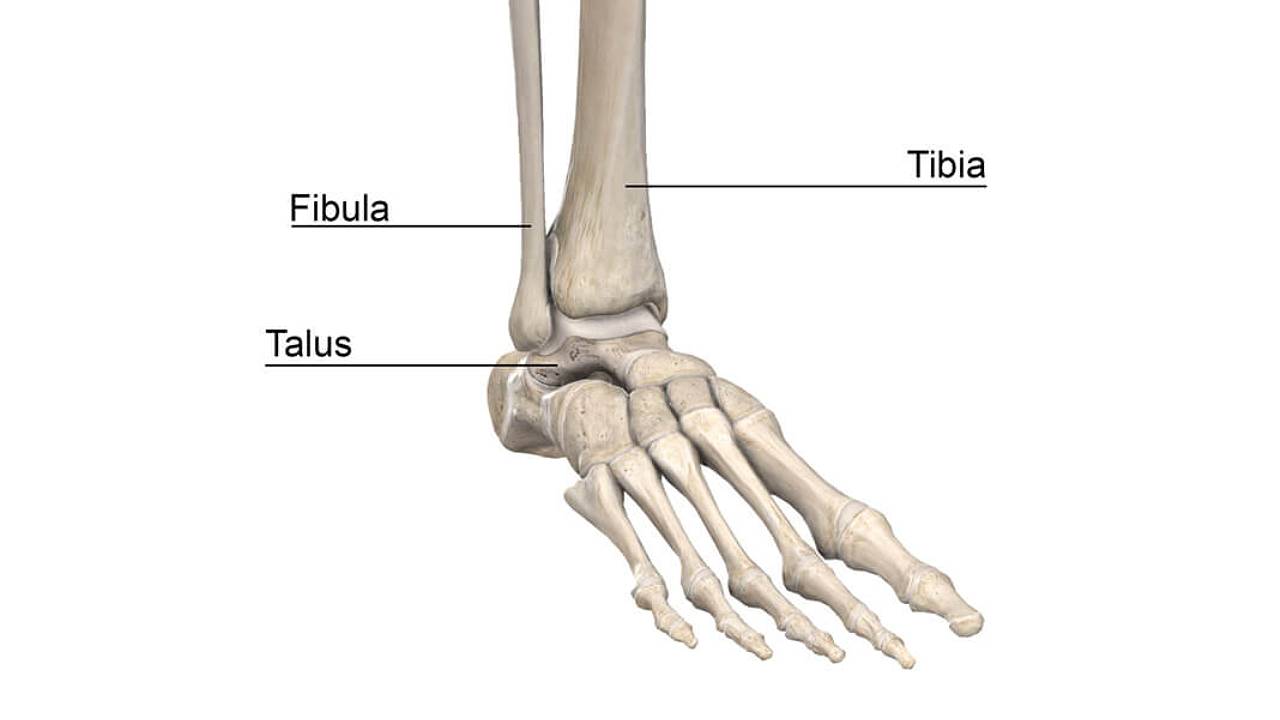
The ankle joint, made up of the talus, fibula and tibia bones, is important in providing support, stability, shock absorption, and balance to a person during ambulation. The ankle joint facilitates smooth motion, enabling an up and down movement. This joint, as many others, is covered with articular cartilage that helps the bones glide smoothly over each other during movement. The cartilage is layered with synovium to lubricate and reduce friction between the bones.
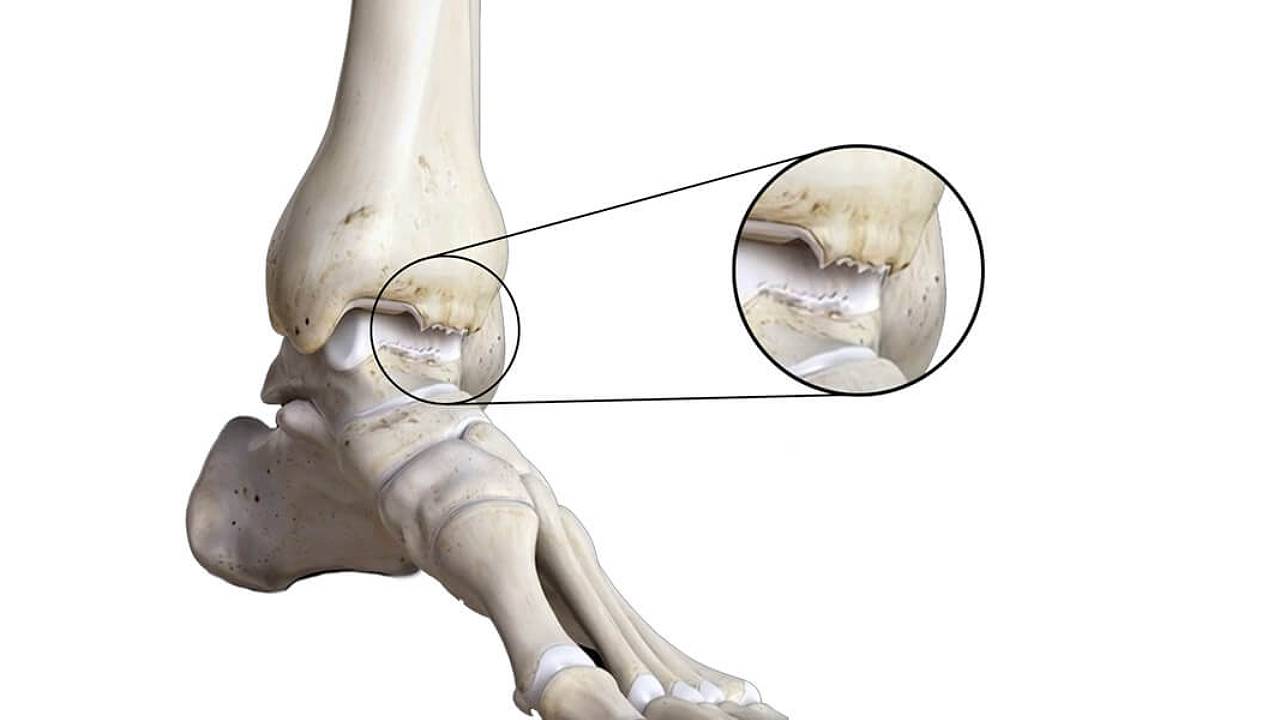
Ankle arthritis occurs when the cartilage of the ankle joint wears away and becomes frayed or rough. This is also accompanied by the narrowing of joint space and the development of bone spurs, known as osteophytes. Some forms of arthritis include:
- Osteoarthritis – cartilage in the joint gradually wears away. Overtime, as the protective space between the bones decreases, the cartilage will become frayed and rough. This can result in bone rubbing on bone, producing painful bone spurs. Osteoarthritis develops slowly, causing pain and stiffness that worsens over time. While previously most common among the aged, it has now become more widely spread amongst younger age groups due to changes in lifestyle. Increased recreational physical activity like high-impact sports or running can cause joint structures like the knee to wear out more quickly, allowing osteoarthritis to set in.
- Post-traumatic Arthritis – this develops after an injury to the foot or ankle. Dislocations and fractures—particularly those that damage the joint surface—are the most common injuries that lead to post-traumatic arthritis, even years after the initial injury. Like osteoarthritis, post-traumatic arthritis causes the cartilage between the joints to wear away. Compared to an uninjured joint, an injured joint is about seven times more likely to become arthritic.
- Rheumatoid Arthritis – this is an autoimmune disease where the immune system attacks its own tissues. In rheumatoid arthritis, immune cells attack the synovium covering the joint, causing it to swell. Over time, the synovium invades and damages bone, cartilage, ligaments and tendons, causing serious joint deformity and disability. This is usually a more aggressive form of arthritis that requires close medical attention with pharmacologic management to reduce inflammation and stiffness, while preventing irreversible deformity..
- Other forms of arthritis – apart from those mentioned above, there are other forms of arthritis that are caused by other underlying conditions, such as metabolic disorders. For example, elevated levels of uric acid (hyperuricaemia) may cause gouty arthritis which affects the joint, causing joint erosion and disability over a prolonged period.
Symptoms
- Painful inflamed joints
- General feelings of being lethargic
- Gradual or sudden onset of pain
- Pain with movement and with specific activities
- Tenderness around joints upon palpation
- Joint warmth, swelling and redness
- Increased pain, swelling or stiffness in the mornings or after resting
- Difficulty in walking
- History of ankle fractures or sprains
- Limping or notable gait changes
- Weakness in the lower limbs

How we can help?
X-rays may be ordered to determine the extent of articular damage. Arthritic ankles may show narrowing of the joint space between bones (an indication of cartilage loss), changes in the bone (such as cysts or fractures), or the formation of bone spurs. Further diagnostic tests may be required including, bone scans, CT or MRI scans and blood tests.
Leaving ankle arthritis to deteriorate often results in chronic pain, disability and deformity of the foot and ankle joint. This makes daily life very difficult for patients due to the gradual loss of mobility. Although there is no cure for arthritis, there are strategies to slow the progression of the disease. Podiatric interventions may include custom orthotics, exercise programmes, and medical technologies, such as Extracorporeal Magnetotransduction Therapy (EMTT). With proper care, many people with arthritis are able to manage their pain, remain active, and lead fulfilling lives.
Lifestyle modification may be necessary:
- Minimising activities that aggravate the condition
- Switching from high-impact activities (like jogging or tennis) to lower impact activities (like swimming or cycling) to lessen the stress on your foot and ankle
- Losing weight to reduce stress on the joints, resulting in less pain and increased function
- Physical activity for strengthening joints and increasing range of motion in the joints




