It has been estimated that 15% of the population will develop foot ulcers in their lifetime. This number then increases to 25% amongst diabetics and is an underlying cause for 84% of all non-traumatic lower leg amputations.1 Consequently, patients in cases of lower extremity amputation often suffer a higher rate of mortality due to marked functional decline within a 5-year-period after the procedure.2
To combat this, a multidisciplinary approach through preventative measures, regular inspection, and early intervention has been shown to reduce a diabetic patient’s amputation rate by up to 50%.3
How Do Diabetic Foot Ulcers Form?
Diabetic ulcers describe wounds that do not heal normally and are at high risk of deterioration and infection due to a multitude of interrelated diabetic complications.
Diabetic foot ulcers typically form due to:
- Overloading of a particular area of the foot
- A small abrasion or blister from unsuitable footwear choices
- Ingrown toenails
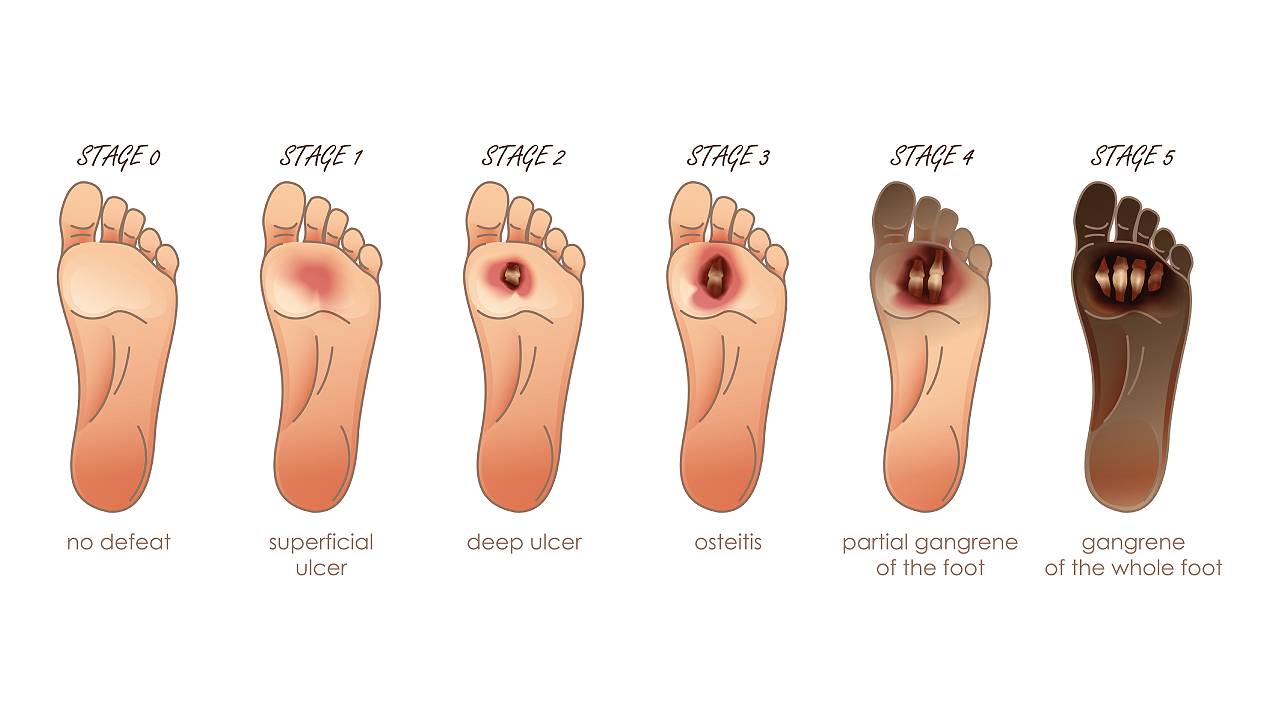
Diabetes can cause many complications such as blindness, kidney failure, and foot ulcerations. Although all these examples are serious, foot ulcerations are likely the most severe complication as they can lead to gangrene or tissue death, or even result in eventual amputation of the limb or death if sepsis develops.
Risk Factors for Diabetic Foot Ulcers and Wounds
- Peripheral neuropathy
- Structural foot deformities (bunions, toe deformities, collapsed foot, Charcot foot)
- Peripheral vascular disease (PVD) / peripheral arterial disease (PAD)
- Lack of compliance to medical advice
- Uncontrolled blood sugar levels
- Trauma to the feet and lower limbs
- Neglected regular inspection of the feet for wounds, skin changes, and infection
- Smoking
Proper patient education regarding foot hygiene, nail care, and footwear choices is crucial to reducing risk factors that can lead to the formation of diabetic ulcers and wounds.

What Can My Podiatrist Do For Diabetic Foot Ulcers and Wounds?
An assessment with a podiatrist will involve a thorough examination and extensive medical history-taking to verify the severity level of your wound. A full diabetic foot examination will be carried out through the use of doppler/ ABPI/ TPBI to check for neuropathy and vascular insufficiency.
Diabetic foot ulcer and wound healing assistance include:
- Wound debridement, cleansing, and care using specialised dressings
- In-clinic wound management with extracorporeal shockwave therapy (ESWT) to promote healing by boosting circulation and rate of tissue formation
- Casting of the lower limb depending as needed (soft, compressive, fixed, removable, fibreglass, plaster of Paris)
- Long-term offloading, footwear modifications, and customised orthotics to prevent wound recurrence

Our podiatrists aim for diabetic patients to be able to resume a pain-free and active lifestyle with a minimised risk of wounds and infections. Regular foot care and wound management are key to stabilising the foot condition and reducing the need for follow-up visits. Twice yearly diabetic foot examinations should be done to track a patient’s foot condition and overall risks, so a wound or ulcer can be detected promptly and prevented from worsening. If a diabetic wound or ulcer has developed, more frequent examinations and interventions will be required to avoid amputation.
If an additional form of management or surgical intervention is required, referrals can be made by your podiatrist to a wide range of endocrinology, orthopaedic, or vascular specialists.
Diabetic foot ulcers and wounds that are not managed promptly can easily become infected and develop into:
- Gangrene: Tissue dies due to lack of blood flow. If left neglected, this may quickly accelerate and lead to amputation.
- Osteomyelitis: Infection of the bone that has spread from another part of the body, causing inflammation or swelling.
- Sepsis: A life-threatening condition where a pre-existing infection triggers a chain reaction in the body, causing rapid organ failure, tissue damage and may even be followed by the patient’s death.
Why Are My Diabetic Wounds Not Recovering?
Lowered sensitivity/diabetic neuropathy
People with diabetes can experience nerve damage, which can lead to numbness. This can make it difficult to feel pain, resulting in foot injuries such as wounds and fractures going unnoticed. Delayed or improper care due to a state of obliviousness is a likely probability as to why a diabetic wound is not recovering.
Poor circulation
Diabetic individuals have narrowed blood vessels which can slow down blood flow and make it difficult for wounds to receive the required oxygen and nutrients for healing. The effectiveness of white blood cells also decreases, leaving them unable to fight off infections.
Poor blood glucose control
Insulin is the hormone that breaks down glucose to use as energy in the body. Diabetes is the result of the body’s inability to produce consistent insulin, making it difficult to manage blood glucose levels. High blood glucose levels over a prolonged period will cause white blood cells in the body, which are an essential part of the immune system, to be unable to function correctly, fight infection-causing bacteria, and close wounds.
Although there is no certain way to cure diabetes, remission is possible with the appropriate management methods. The patient should be responsible for their lifestyle modifications, pharmacotherapy, glycaemic control, and the prevention and management of associated conditions. Furthermore, a reputed medical practitioner with good references to other diabetic specialists should be consulted to drastically increase the chances of success.
How Do I Speed Up The Healing of My Diabetic Wounds?
Healthy diet
Diet and blood sugar levels are closely linked, and this can have a nonlinear impact on the rate of recovery. People with diabetes should avoid carbohydrates, processed foods, added sugars, and fast food. They should focus on eating foods high in protein, fruit, vegetables, and legumes. A healthy diet can help keep blood sugar levels consistent, improve overall nutrition, and speed up the recovery process. Specialised podiatric methods such as radial shockwave and SIS can also help a patient improve recovery.
Stay active
Regular exercise promotes good blood flow and improves the rate at which sugar in the bloodstream enters cells. This aids in the rate of healing.
Quit smoking
Smoking disrupts the immune system and puts a diabetic individual at a higher risk for many health conditions. This habit also inhibits the ability of red blood cells to bind to and carry oxygen around the body, resulting in impaired healing of injured tissues.
Keep pressure off the affected area
Consistent pressure on a diabetic ulcer can damage the skin further and lead to deeper wounds.
Regular dressing changes
Through the proper maintenance of wounds and the use of special wound care dressings, moisture levels in the wound will be retained and chances of infection are decreased.
Visit a podiatrist for specialised advice on diabetic wound care. If you have a diabetic ulcer, seek medical care immediately as early intervention can improve chances of healing, avoid the onset of infection and complications, and prevent amputation.




