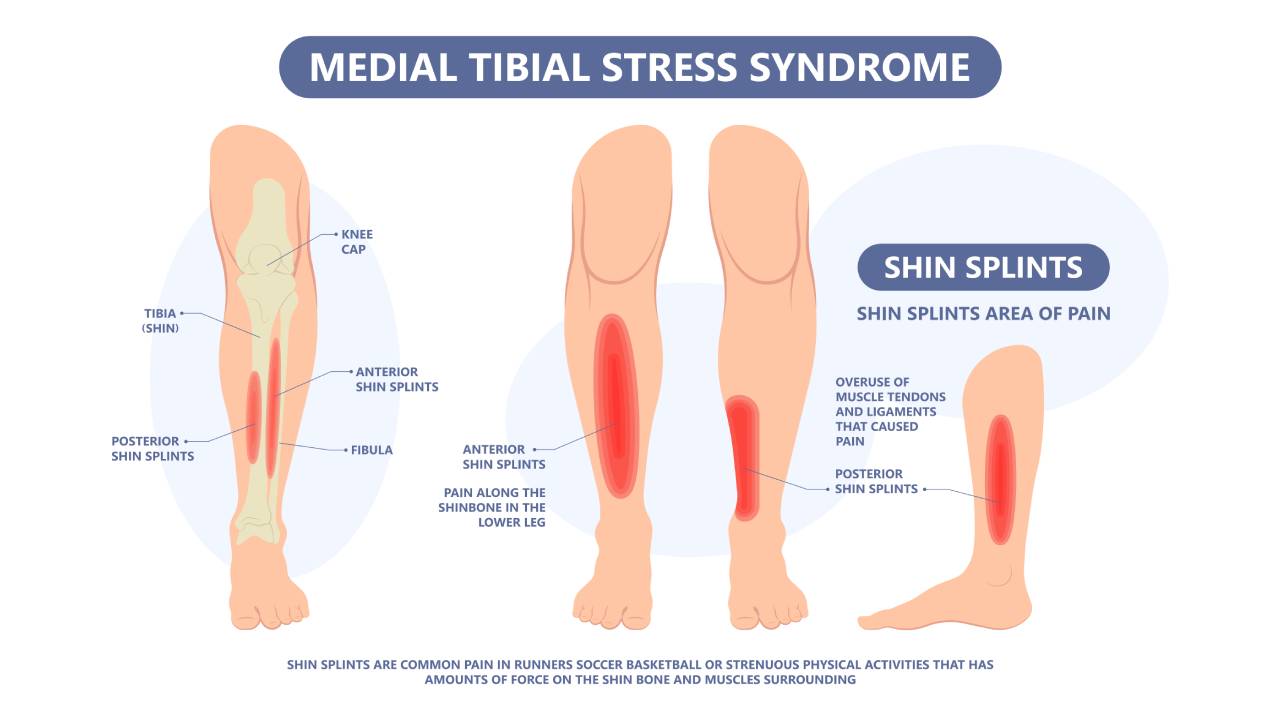
Medial Tibial Stress Syndrome (MTSS), more commonly known as shin splints, is an overuse injury of the lower leg musculature. Shin splints typically occur when too much stress is localised at the tibia (shin) bone, causing inflammation and pain in the muscles, tendons, and periosteum (bone lining).
Typically, this occurs when there is an increase in physical activity, leading to the musculoskeletal tissues becoming overworked. Serious complications, such as tibial stress fractures or chronic compartment syndrome will be the result if shin splints are not diagnosed and managed early. These complications may require orthopaedic or reconstructive surgery.
Causes of Shin Splints
Shin splints are often caused by a sharp increase in physical intensity or volume of exercise, such as working out after a long period of inactivity. This sudden burst of activity causes the muscles around the tibia bone to become overused and fatigued, resulting in pain.
Other common factors contributing to shin splints are:
- Overpronation
- Flat feet
- Unsupportive footwear
- Inadequate muscle stretching
- Activity-specific ground surface density
Individuals at a higher risk for developing shin splints include runners, military personnel, active sportspeople, and dancers.

Signs and Symptoms of Shin Splints
- Pain at the inside edge of the tibia (shin bone)
- Pain that is aggravated by manual pressure
- Sharp, or dull and aching pain
- Pain during or after vigorous activity
- Tingling and numbness radiating from the shin to the foot
What to do if you suspect that you have shin splints?
The first line in managing shin splints is to stop all physical activities, get sufficient rest, and ice the affected area to reduce pain and inflammation. If the pain does not subside after a few days, or if it is recurrent, it will be time to see a podiatrist. Shin splints can also be a symptom of other, more serious conditions, such as tendonitis, longitudinal tendon tears or stress fractures.
A musculoskeletal assessment, physical examination, diagnostic ultrasound, and X-ray may be ordered to ascertain an accurate diagnosis. After a thorough assessment, your podiatrist will be able to recommend a suitable plan to resolve your shin splints.
Non-invasive methods your podiatrist may use include:
- Super-inductive therapy (SIS)
- Focal and radial extracorporeal shockwave therapy (ESWT)
- Stretching exercises
- Custom orthotic insoles
Shin splints can become more painful and persist over time if not managed properly. The main risks associated with shin splints are stress fractures, nerve pain, and muscle compression. If the pain becomes more noticeable or does not improve, it is important to seek a foot specialist or podiatrist promptly.




