Aging is associated with a decline in muscle strength and level of activity, which can lead to an increased risk of falls due to the lack of lower limb strength. One in three people aged 65 and above, and one in two aged 80 and above will experience a fall at least once per year, with at least 40% of all falls in Singapore linked to injury-caused deaths.1
In many circumstances, prior experiences can lead to a fear of falling, causing many elderly to further reduce their level of activity to prevent reoccurrences. Therefore, the improvement of functional mobility, and reduction of muscle weakness and gait deficits, is key to promoting strength and balance in the elderly and improving their quality of life.
Conditions That Can Impact Strength and Balance
The ability to remain upright requires intricate neuromuscular control (the relationship between the nerves and muscles). This depends on the body’s reaction to sensory input which impacts the brain and nerves such as vision, hearing, and sensation in the extremities, providing us with the proper muscular control to respond to potential hazards. However, a delayed reaction can occur if any part is slow to respond to stimulation, especially if the patient has prior impairments that can affect movement.
Many lower limb conditions can lead to mobility issues and increase the risk for falls, with the most common being:

- Diabetic-related lower limb issues
- Balance and gait impairments
- Osteoporosis or osteoarthritis
- Fractures from previous falls
- Foot problems (bunions, calluses, corns, etc.)
In some cases, elderly patients often do not report previous falls, pre-existing injuries or other health conditions. Failure to reveal such information can lead to the issue worsening or becoming chronic, and can lead to a further increased chance of falls. Therefore, already weakened individuals have their problems rectified at the source to prevent a cycle of falls from developing.

How Can Your Podiatrist Help?
Podiatrists are experts trained to address conditions causing pain, weakness, and immobility in the lower limbs. This is accomplished through the use of rehabilitative non-invasive therapies such as the Super Inductive System (SIS) and prescription custom foot orthotics.
The Super Inductive System (SIS) and Extracorporeal Magnetotransduction Therapy (EMTT) are commonly utilised to rehabilitate neuromuscular and joint-skeletal disorders through the use of an electromagnetic field. This causes the depolarisation of neuromuscular tissues and induces muscle contractions. As a result, joint mobilisation, muscle strengthening, and fracture healing can be achieved at a much faster rate.
Custom foot orthotics are specialised devices that are prescribed after a comprehensive biomechanical and gait assessment to determine if the patient is suitable. They can provide your feet with the proper structural support to lessen pain and offer correction of foot conditions through realignment. Such conditions can include foot deformities such as bunions, calluses, lesser toe deformities, and corns. These are proven to cause impediments to movement and are also associated with decreased functional ability and balance deficits. In addition to correction of deficits, customised foot orthotics also improve propulsion and proprioception in those with sensory deficits.

Your podiatrist can also provide general nail and maintenance services for elderly patients with toenail deformities, and who might not be able to clip them on their own. Not only does this reduce the reoccurrence of future nail deformities such as ingrown toenails, but it will also help boost overall mobility by ensuring pain-free feet. Such visits are also useful for monitoring elderly foot health, particularly for signs of nerve degradation or decreased sensitivity to pain or sensation, reducing the risk of falling due to a lack of proprioception.
When Should I See a Podiatrist?
Keeping an elderly patient sedentary for prolonged periods can hinder and delay their recovery. If you or someone you know has just suffered from a fall, approach a podiatrist to help lessen pain through the use of advanced technologies that target the injured tissue. This helps accelerate the rate of healing so patients can return to their daily activities as soon as possible, and by doing so, promotes activity and movement.
Reducing aching joints and tendinopathies ensures that movement is pain-free and encourages a stable and balanced walking pattern which would minimise the risk of falls.
What Can the Elderly Do at Home to Improve Strength and Balance?
Balance exercises
Physical activity can improve flexibility, coordination, and posture, increasing stability and greatly reducing the risk of falling. It is important that the elderly feel confident in their movements so they will have the motivation to be more active.
Strength training
The decline of muscle strength as one ages is a natural process that cannot be reversed, but it can be slowed down. Specific exercises targeting the muscles can significantly reduce the chances of developing osteoporosis or other cardiovascular disorders.
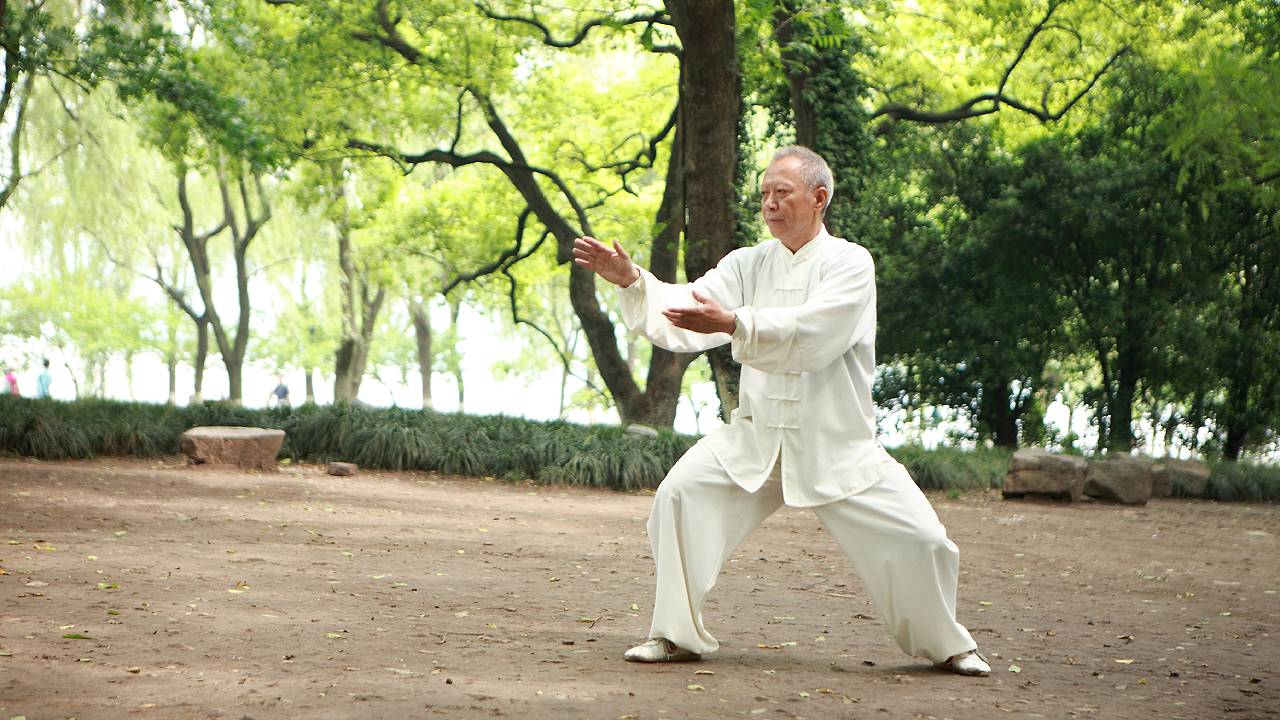
One example of an all-rounded workout routine is taichi, which encompasses cardiovascular, strength, balance, and flexibility exercises.
It is recommended to consult with a professional before starting any new exercises. Make it a point to do physical activity every day; start with easier exercises before moving on to more challenging ones, and be sure to take breaks when needed. Furthermore, aside from the physical benefits, exercise also helps to improve mental health and can be a great opportunity to interact with others.
Nutrition
A balanced diet is important as weight gain can affect strength and balance, particularly for the elderly. There should be careful consideration for healthier options such as relying on foods like lean meat, fish, poultry and eggs as sources of protein. Vitamins and health supplements like calcium and vitamin D are also encouraged but care should be taken as some elderly patients may have trouble chewing and swallowing. However, as the recommended level of nutrition and diet requirements vary widely from person-to-person, it is advised to check with your doctor or nutritionist on the appropriate foods before changing your diet plan.
Improving strength and balance in the elderly starts from the bottom up. Ensuring the well-being of lower limb health and addressing past injuries are crucial in maintaining healthy mobility amongst older adults. This in turn minimises the risk of falls and further complications, improving their overall quality of life.
If you or any of your family members are experiencing pain from fall-related injuries or are worried about underlying lower limb conditions, make an appointment with a podiatrist today.




