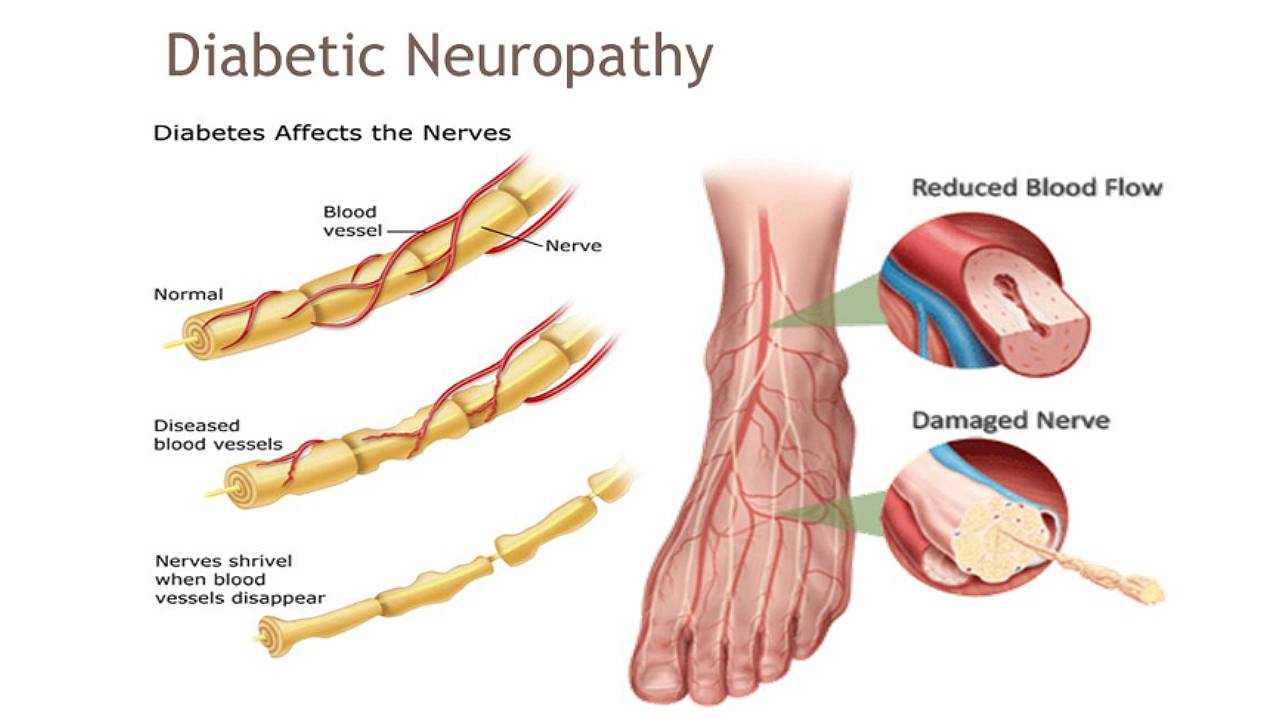
Diabetic neuropathy is a complication of diabetes that results in damage to the nervous system. Nerves are essential to a functioning body as they control sensation, movement, and unconscious movements like breathing and heartbeat regulation. Nerve damage in any area of the body causes the loss or reduction of control signals and can get progressively worse over time.
How Does Diabetic Neuropathy Affect Me?
Early stages of nerve damage may not have any obvious signs or symptoms. As the damage progresses, a person suffering from diabetes may experience burning pain, tingling sensations, a loss of tactile sensation in the feet and hands. Due to this loss of sensation, any injury sustained (i.e. a cut on the foot, development of a blister, an inflamed ingrown toenail, etc.) may not be noticed in time.
An unresolved wound can fester and develop an infection that can spread quickly, leading to gangrene, a serious condition that can be fatal. This condition can spread to other parts of the body and cause sepsis, a life-threatening blood infection. This leaves diabetic patients an increased risk of amputation of affected limb, as their blood sugar levels can make it difficult for the body to fight off infections.
Neuropathy falls into four main categories:
- Peripheral symmetric neuropathy: This affects the nerves in the feet first, and then the hands. It is the most common form of diabetic neuropathy.
- Autonomic neuropathy: This occurs in the nerves that control involuntary body functions such as digestion, urination, and heart rate.
- Thoracic and lumbar root, or proximal neuropathy: This damages nerves along a specific distribution such as the chest wall or legs.
- Mononeuropathy: This affects a single individual nerve, resulting in pain in a localised area, loss of movement, or numbness.
Patients with diabetes can experience multiple types of neuropathy at the same time. Peripheral neuropathy and mononeuropathy are the two most common forms of neuropathy that podiatrists see in diabetic patients.
What Are The Symptoms of Diabetic Neuropathy?
Symptoms of diabetic neuropathy build up over time, and commonly affect the feet and lower legs first, such as:
- Numbness in the feet and hands in a “stocking-glove” distribution
- Abnormal or altered sensation in hands or feet
- Constant pain in the extremities
- Loss of balance
- Difficulty walking without wobbling
- Loss of muscle tone in the hands and feet
- Inability to feel differences in temperature or physical injuries in the limb
- Tingling or burning sensations radiating from the toes to the ankles (then up the legs over time)
- Bone deformity or foot collapse (Charcot arthropathy/ diabetic foot deformity)
Diabetic neuropathy worsens with time without the proper regulation of lifestyle choices such as reducing sugar and fat intake. Patients that do not develop any abnormal pains will still face a greater risk of falls if the early signs of diabetic neuropathy such as impaired balance and loss of sensation in the outer extremities are not addressed.

How Do Podiatrists Manage Diabetic Neuropathy?
There is currently no cure for diabetic neuropathy, but there are remedies that can help to slow down the progression of the disease, solve any secondary conditions, and relieve pain. Patients find that dedicated and targeted intervention methods can reverse damage and are useful in re-establishing sensations. However, this can vary depending on factors such as glucose control, vascular supply, and the degree of nerve deterioration.
Your podiatrist will carry out recurrent comprehensive diabetic foot-specific examinations to ensure sensation and blood flow to the feet are not in rapid decline. They will also take care to check for the presence of any subsequent secondary conditions.
Podiatric solutions for diabetic neuropathy include:
- Preserving the shape and function of the feet, reducing fall risk, and preventing the deformation and collapse of diabetic feet with custom foot orthotics or ankle foot orthotics (AFOs). This helps patients remain active and mobile.
- In-clinic therapy with Super Inductive System (SIS) and Extracorporeal Magneto transduction Therapy (EMTT) to reduce the tingling, numbness, and burning sensations while increasing localised blood supply.
- A prevention and wellness management plan which includes skin, nail, and specialised wound care to help the patient avoid limb amputation as much as possible.
How Do I Prevent Diabetic Neuropathy?
Lifestyle changes
-
Weight management
Maintaining a healthy weight decreases the occurrence of diabetic symptoms and makes it easier to control blood sugar levels. This greatly reduces the risk of a diabetic person developing neuropathy or other complications.
-
Quit smoking
Smoking damages blood vessels and impacts blood flow in the body, affecting various body parts. It also raises blood glucose levels, makes it harder to control blood sugar, and increases the likelihood of secondary conditions such as heart disease, eye problems, or stroke.
Maintain blood sugar level
The risk of developing diabetic neuropathy increases, the longer a person has diabetes. This is because high blood sugar levels over long periods of time can cause significant nerve damage, resulting in the onset of diabetic neuropathy symptoms.
Prevention is key to managing diabetes. At-risk diabetic patients should see a podiatrist every 3 to 6 months for any foot abnormalities. Low-risk diabetic patients should be seen yearly if there are no major concerns with their feet and lower limbs.




