Peripheral vascular disease (PVD) is an umbrella term describing generalised blood circulation disorders that cause blood vessels to narrow, spasm, or become blocked. These diseases can affect the arteries, veins, and lymphatic vessels.
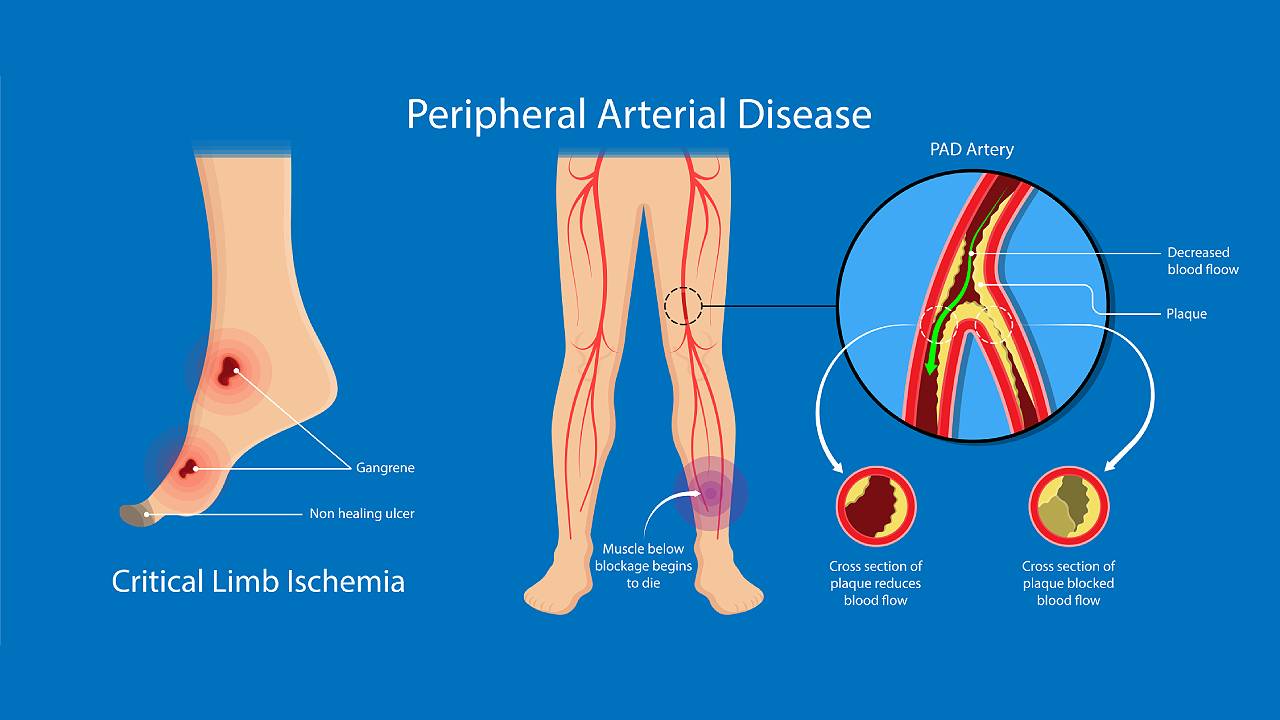
Peripheral Arterial Disease (PAD) develops only in the arteries and primarily affects the ones in the legs. PAD usually arises due to the build-up of plaque in the arteries and restricts the amount of oxygen and nutrients needed by the body to stay healthy.
There are numerous risk factors for PVD/ PAD such as:
- Being above the age of 50
- Obesity
- Comorbidities (high cholesterol, previous stroke, heart disease, high blood pressure, diabetes, kidney disease)
- Sedentary lifestyle
- Poor eating habits
- Smoking
- Drug use
- Emotional stress
- Extended exposure to cold temperatures
What Are The Symptoms of Peripheral Vascular Disease and Peripheral Arterial Disease?
PVD/ PAD are not signs of aging but progressive conditions that start slowly and develop into serious underlying medical conditions. The two conditions can be difficult to tell apart due to their similar symptoms but there are subtle differences. These symptoms include:
| Peripheral Vascular Disease | Peripheral Arterial Disease |
|---|---|
|
|
Claudication is a typical shared symptom of PVD and PAD. This refers to the onset of muscle pain and fatigue due to a lack of oxygen in the blood vessels from physical activity, but abates promptly with rest.
As the condition worsens, symptoms will occur more frequently and get worse. The individual may even experience pain and fatigue during rest.
Unresolved PVD and PAD can cause an affected limb to develop non-healing wounds and eventually become gangrenous. If the disease has progressed to this stage, limb amputation is typically necessary to stop tissue death from spreading.
How Can A Podiatrist Help With PVD/PAD?
Podiatrists are often the first to detect abnormalities in the lower limbs that may be indicative of PVD/PAD. If your podiatrist suspects PVD/PAD, they will perform vascular supply screenings such as Doppler ultrasound or Ankle Brachial Index (ABI), to obtain an accurate diagnosis. An early diagnosis is essential to preventing many life-threatening complications.

Our podiatrists can assist with:
- Swift assessment and diagnosis
- In-clinic therapy for the improvement of microcirculation when appropriate
- Specialised care for high-risk feet to reduce the risk of wound development
- Specialised wound care for skin ulcerations
- Dispensing advice on how to keep physically active
- Timely referrals for surgical evaluation
- Post-amputation wound care and assisted return to mobility
If the diagnosis and interventions are delayed, it can lead to further complications and reduce the chances of successful outcomes. In some cases, these complications can lead to the development of different types of gangrene.
| Dry Gangrene |
|---|
|
| Wet Gangrene |
|---|
|
| Gas Gangrene |
|---|
|

The sudden development of a cold, painful, pale limb with a weak or no pulse is classified as a medical emergency and will prompt your podiatrist to refer you for an emergency vascular assessment immediately. The loss of oxygenated blood to a limb or area of the body will cause significant tissue death and can leave patients fighting for their lives.
The main goal of podiatry is to prevent the need for amputation. If amputation does occur, then the aim will be shifted to helping the patient avoid further tissue loss and additional amputation.

If you or a loved one suspect the presence of arterial issues affecting the lower limbs, please do not hesitate to seek a professional opinion. An in-clinic vascular screening should be carried out as soon as possible to slow symptoms down and prevent the need for amputation.




