
Singapore’s weather of rain and humidity can have many effects on the feet; creating optimal conditions for fungus to spread in the skin and toenails. Undetected to the naked eye, fungal spores are opportunistic in nature and latch onto any possible host. They thrive in moist environments, causing itchiness, flaking, red spots and dryness to the skin of the foot.
If a fungal skin infection worsens, it can lead to a condition called foot rot. This is a bacterial infection that develops on top of the fungal infection, often causing bleeding, pus, open wounds, and pain. If ignored or incorrectly managed, foot rot can become a medical emergency. It is also contagious and can be transmitted to close contacts.

Fungal nails and skin fungus are closely related. If you have a chronic fungal skin infection, you’re more likely to also have a fungal nail infection, or vice versa.
Fungal nails can appear in many different ways. Superficial fungus appears as a white or yellowish discolouration on the top surface of the nail.
Over time, the fungus can invade the underlying nail bed, causing the nails to become thick, crumbly and lifted. The nail may appear dark yellow, brown, greenish or white.
Once nail fungus invades the nail bed, it can be difficult to manage and eliminate. Leaving the fungus unaddressed can allow it to spread to all ten toenails, as well as to others around you.

Self-Monitoring & Prevention
Prevention is important. Ensure the feet are always dry, especially in between the toes. Rotate the use of footwear regularly, allowing aeration of the shoes. Wear socks with closed footwear at all times, and change them at least once or twice daily. Avoid sharing nail clippers, files, polish or other products with other people. Refrain from salon pedicures as cross-contamination can occur if the instruments are not properly sterilised; some pedicure enthusiasts prefer to bring their own instruments to their salons. Most importantly, pay good attention to the state of your feet and nails by checking them daily.
If you notice changes or discolouration to your nails or skin, it may be a sign of a fungal infection. However, many other conditions can have similar appearances, such as psoriasis or even skin cancer. It is essential to get a proper diagnosis of the condition to ensure that you receive the correct management and care.
Close monitoring by a healthcare professional can help ensure that the problem addressed properly.

Realities of Over-the-counter Antifungal Products
Home remedies are mostly not strong enough to eradicate stubborn nail fungus. There is a variety of over-the-counter options claimed to be effective for resolving nail fungus. Tea tree oil, apple cider vinegar and more, are common items which many patients have tried in order to eliminate nail fungus. These products often do not have strong antifungal ingredients. The infection may seem to clear up for a period of time, but the chances of recurrence are very high.
Over-the-counter antifungal products can be effective for mild or superficial nail fungus, but they require consistent and diligent application for at least 6 to 18 months. Topical products come in various forms such as ointments, creams, drops and lacquers. However, they have minimal or no effect for severe infections, as the fungus may have invaded the deeper layers of the nail plate, nail bed, or even the nail matrix (nail root).

Clinical intervention Options for Nail Fungus
It can be an uphill battle in Singapore’s climate, yet fungal nails can be managed well if intervention is prompt. Chronic fungal infections can be managed with oral antifungals. Oral drugs such as terbinafine (Lamisil) and itraconazole (Sporanox) are commonly prescribed. They act to help healthy nail grow out from the nail matrix in replacement of the infected ones. A minimum course of three months is usually needed to improve or resolve the condition. Because oral antifungals are potent drugs, the most significant side effect is liver toxicity.

Hence, monthly blood tests are required to monitor the patient’s liver function. Oral antifungal medications can also interact with anti-depressants and beta-blocker medications. Patients with liver and heart problems are usually contraindicated for this intervention method.

With the advancement of medical technology, laser and light therapies have become more common in recent years. They have proven to be effective with little to no side effects.
Patients have found a preference for this approach as it avoids the disadvantages of oral and topical drugs while providing relatively fast results.
Photodynamic Antimicrobial Therapy (PACT) is one such approach offered in our practice: Fungal cells possess a cell wall, unlike human cells. A photosensitizing gel specifically targeting fungal cell walls is applied to the nail, causing the fungus present to be vulnerable to a specific wavelength of light. Direct exposure to the specific light then destroys the stained fungus, even those which have become resistant to the strongest antifungal medications. Just like a course of antibiotics, a number of sessions are required for effectiveness. Top-up sessions may be required depending on the progress.

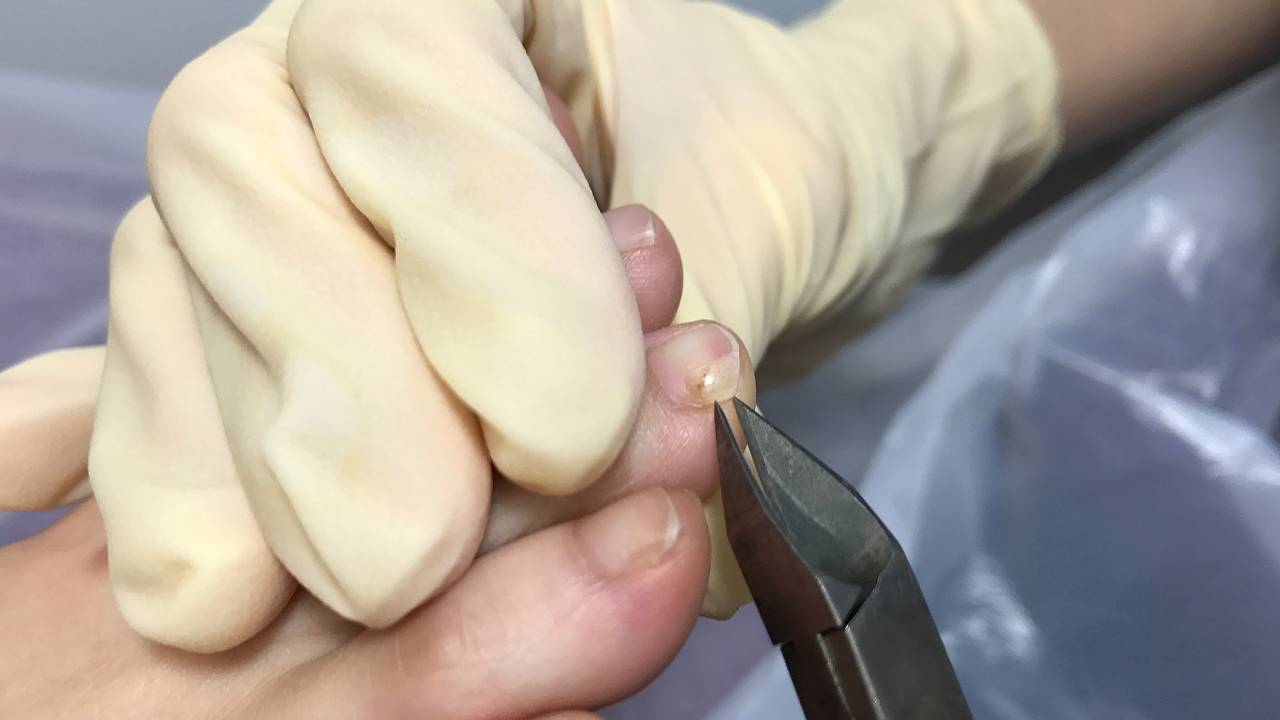
A surgical option for resolving fungal nails is often used when the entire nail bed has been deeply infected by fungus. Surgically removing the entire nail plate is known as a total nail avulsion. This is carried out to achieve a “blank canvas” for the nail bed, giving a new nail the best opportunity to grow out clear and fungal free. Healing time for the surgical wound usually takes one to two weeks. As part of this fungal nail management, immediately after the wound is healed the patient is required to follow through with a course of PACT therapy to ensure that fungal spores are completely eliminated from the nail bed.

There are many options to consider. Patients hoping to be free of stubborn fungal infections should dedicate full compliance once therapy has started, in order to ensure success. Eradicating fungus is often not 100%, especially in Singapore’s tropical climate. Without proper clinical care, there is a high possibility of re-infection. Timely podiatric care is key to preventing the spread of fungus from toenail to toenail.




